Wendy Earthsong, BA, CCS-P, CHPS, is an Associate Professor in the Medical Coding program at Everett Community College
I am a professor in a Medical Coding/Billing program at a community college in Washington state. My experience in the healthcare field began as a certified nursing assistant. I transitioned to management and administration of healthcare clinics. Later, I took my clinical and administrative skills into higher education and started teaching future medical assistants and health information management professionals.
Throughout my career as a healthcare administrator and educator, I have addressed a recurring theme from healthcare students and staff alike. That is the idea that, by choosing to work in the administrative side of the healthcare house, they “won’t have to deal with patients.” I steer people away from this perspective as quickly as possible.
This limited view of the role an administrative staff member plays when performing their tasks and duties is not only incorrect, it is also part of the problem with patient satisfaction in healthcare today.
Simply put, the healthcare encounter is not solely the time spent with the provider and clinical staff. In truth, the encounter is the entirety of the interactions between the patient and the healthcare system.
If we consider our own experiences with the healthcare industry, we can readily attest that any step in those myriad interactions throughout a healthcare encounter can affect not only the mindset of the patient but also the outcome of care for the patient.
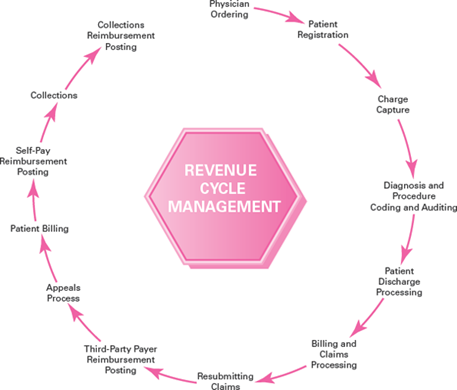
The revenue cycle model offers clarity to healthcare students
Any revenue cycle model supports the fact that, for the majority of healthcare encounters, administrative staff members interact with the patient more than clinical staff do.
This interaction is not always face-to-face and is not direct care in nature. Administrative tasks and functions precede the clinical care and proceed through and beyond clinical care.
When any member of the healthcare workforce fails to understand that they, too, are impacting patient care and patient outcomes, the system at-large fails the patient/client/resident.
Healthcare students and staff alike must understand from the outset that we all deal with patients.
I believe that we, as instructors in educational programs tasked with training students for success in administrative healthcare jobs are responsible for challenging our students to understand the full scope of their role in healthcare―and their full impact on the lives of each individual patient whose information they touch.
We have a big mandate in our teaching careers. We must cover the broad scope of knowledge, skills, and abilities healthcare students need for successful completion of their coursework and successful beginnings to their careers. And, if we consider the big picture, we must strive to improve healthcare one student at a time.
The most important member of the healthcare team
We talk about internal and external stakeholders, the importance of data integrity, information governance, the revenue cycle, communication, and interaction with stakeholders. What’s more, we address the issue of teamwork in our courses. As we deliver countless lectures, discussions, assignments, quizzes, and exams, how many of us emphasize the most important team member of all? The patient!
The patient/client/resident is the only reason the healthcare industry exists. One of our most important overarching mandates as educators must be to make this clear to our healthcare students. To teach our students how to share in the quality healthcare experience for each patient. How to include the patient in a very authentic way on the team. And in turn, how to support and promote patient satisfaction.
In fact, The New England Journal of Medicine article, “Patient Satisfaction Survey,” states “Although, not everyone agrees on exactly what or how to measure it, patient satisfaction has become an integral part of the current health-care delivery system.”
From a clinical perspective, there is a focus on “the delivery of essential medical care; treatments sought by patients and their families (which may or may not be favorable to good health); and the provider activities and behaviors that comprise compassionate care and the safeguarding of human dignity.”
From an administrative perspective, we know patient satisfaction, outcome measurements, and quality care measurements ultimately impact the reimbursement received for care rendered. The PubMed article, “The Role of Patient-Reported Outcome Measures in Value-Based Payment Reform,” states “Pressure to improve the quality of patient care and control costs have caused a rapid shift from traditional volume-driven fee-for-service reimbursement to value-based payment models.”
It’s healthcare, folks―we don’t make purple widgets
Medicine is a needs-based human-to-human business. As I’ve told countless healthcare students, co-workers, staff, and providers in my 30+ year career: We do not make purple widgets here, folks! We help people. On all levels, in all jobs in the healthcare industry, that is the ultimate mandate.
As an educator working with students seeking careers in administrative positions in healthcare today, how will you provide students with a strong foundational understanding of the critical role they will play? How will you teach them that they will “deal with patients”, that they can, and will impact patient care and outcomes?
Get started with healthcare learning materials that cover patient interactions and patient support.